Gum Disease: Symptoms, Causes and Treatments
The early-warning symptoms of gum disease (periodontal disease), such as gingivitis, alert you to act quickly to prevent the pain and expense of more advanced problems.
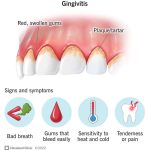
Gingivitis, or inflammation of the gums, is the mildest form of gum disease and exhibits these symptoms:
- Red, swollen and tender gums
- Gums that bleed when you brush or floss your teeth
- Bad breath (halitosis)
Gingivitis can be easily treated. The bone and connective tissue that hold your teeth in place haven’t been affected and the damage to the gums can be reversed. Healthy gums ensure that your teeth are still firmly planted in their sockets.
Gingivitis can mask receding gums, a more serious form of gum disease.
SYMPTOMS OF PERIODONTITIS GUM DISEASE
Gingivitis can worsen into periodontitis, a far more serious gum disease. Periodontitis occurs when bacteria-filled plaque spreads and grows below the gum line. The gums become irritated by the toxins produced by the bacteria. The toxins stimulate a chronic inflammatory response that causes the tissues and bone that support the teeth to be broken down and destroyed.
There are several types of periodontitis gum disease:
- Aggressive periodontitis – This occurs in people who are otherwise clinically healthy. Common symptoms include rapid detachment of gums from teeth and bone destruction.
- Chronic periodontitis – Gum disease symptoms of chronic periodontitis include deep pocket formation and/or recession of the gingiva. Symptoms generally worsen more slowly than in cases of acute periodontitis.
- Periodontitis as a manifestation of systemic diseases – Heart disease, respiratory disease, and diabetes are associated with this form of periodontitis, which may begin at a young age.
Symptoms of the destructive nature of periodontitis include:
- Receding gums – The gum line begins to pull away from the teeth, exposing more of each tooth and eventually the roots, too.
- Deep Pockets – Periodontitis causes the gums to detach from the teeth, creating gaps (pockets) where bacteria collect and grow.
- Loose or shifting teeth – As periodontitis advances and causes more gum tissue and bone loss, teeth begin to loosen and shift.
- Changes in the way teeth fit – The way teeth fit together upon biting down or in the fit of partial dentures may change due to weakness.
CAUSES OF GUM DISEASE
Gum disease happens when plaque builds up around teeth that aren’t cleaned properly. This may be more likely to happen if you find it difficult to clean your teeth well, for example if you wear braces or dentures, or have irregularities in your teeth that you can’t reach with a toothbrush.
There are other factors that can make you more likely to get gum disease, such as:
- Poor Oral Hygiene Habits – This is the most common cause of gum disease. If you don’t brush and floss daily, plaque builds up on your teeth. Plaque is a biofilm that consists of bacteria and the sticky substances they excrete. Daily cleaning and flossing will normally remove plaque. But when the harmful bacteria are left to accumulate on your teeth, the plaque hardens into tartar, a substance that can only be removed by your dentist or dental hygienist.
- Use of tobacco products – Tobacco use may be one of the most significant risk factors in the development and progression of periodontal disease.
- Certain medications – At every check-up, a dentists inquires about medications to determine whether a patient’s usage may have a negative effect on oral health.
- Genetics – Perhaps 30% of the population may be genetically susceptible to gum disease, making them six times more likely to develop gum disease.
- Hormonal changes in women – Significant events in a woman’s life, such as puberty, pregnancy and menopause, can cause hormonal changes that make the gums more susceptible to periodontal disease
- Grinding and clinching teeth – This habit can put too much pressure on the teeth and gums and accelerate or cause gum disease.
- Crooked teeth or misaligned bite – Teeth that bite improperly or are poorly aligned may place too much pressure on certain teeth and gum areas, which may accelerate or cause gum disease.
DIAGNOSIS OF GUM DISEASE
Gingivitis can usually be diagnosed just by your dentist looking at your teeth. But if your dentist thinks you have periodontitis, he or she may look at your mouth more thoroughly and check for gum disease using a periodontal probe. This is used to measure how far your gum has pulled away from your teeth and how much bone – if any – has been lost. Your dentist will do this by putting the probe beside each tooth and underneath your gum line to check how well your gums are attached to your teeth.
You may also need to have X-rays to check the condition of your teeth and jaw bone.
TREATMENTS OF GUM DISEASE
The first line of treatment for gum disease is a deep cleaning procedure called scaling and root planing. This involves removing the plaque and tartar that has built up on the teeth and root surfaces, and smoothing out any rough areas on the roots to help the gums reattach to the teeth. The procedure is usually done under local anesthesia to ensure patient comfort. After the procedure, the dentist may prescribe antibiotics to help control the infection.
In more advanced stages of gum disease, surgery may be required to clean out the pockets around the teeth or to graft new tissue onto the receding gums. There are several surgical treatments available, including flap surgery, bone grafting, and guided tissue regeneration. Flap surgery involves lifting the gums back to remove the tartar and bacteria from the pockets, then reattaching the gums in a new position to reduce the pocket size. Bone grafting involves adding new bone to the area to replace the bone that has been destroyed by the infection. Guided tissue regeneration involves placing a special membrane between the gum and bone to encourage new bone growth and prevent the growth of bacteria.
In extreme cases, tooth extraction may be necessary if the tooth is too damaged or cannot be saved. In this case, the dentist will remove the tooth and recommend replacement options, such as dental implants, bridges, or dentures.
In addition to these treatments, it is important to maintain good oral hygiene habits to prevent gum disease from recurring. This includes brushing twice a day, flossing daily, and using an antiseptic mouthwash. Regular dental check-ups and cleanings are also essential to detect and treat gum disease early.