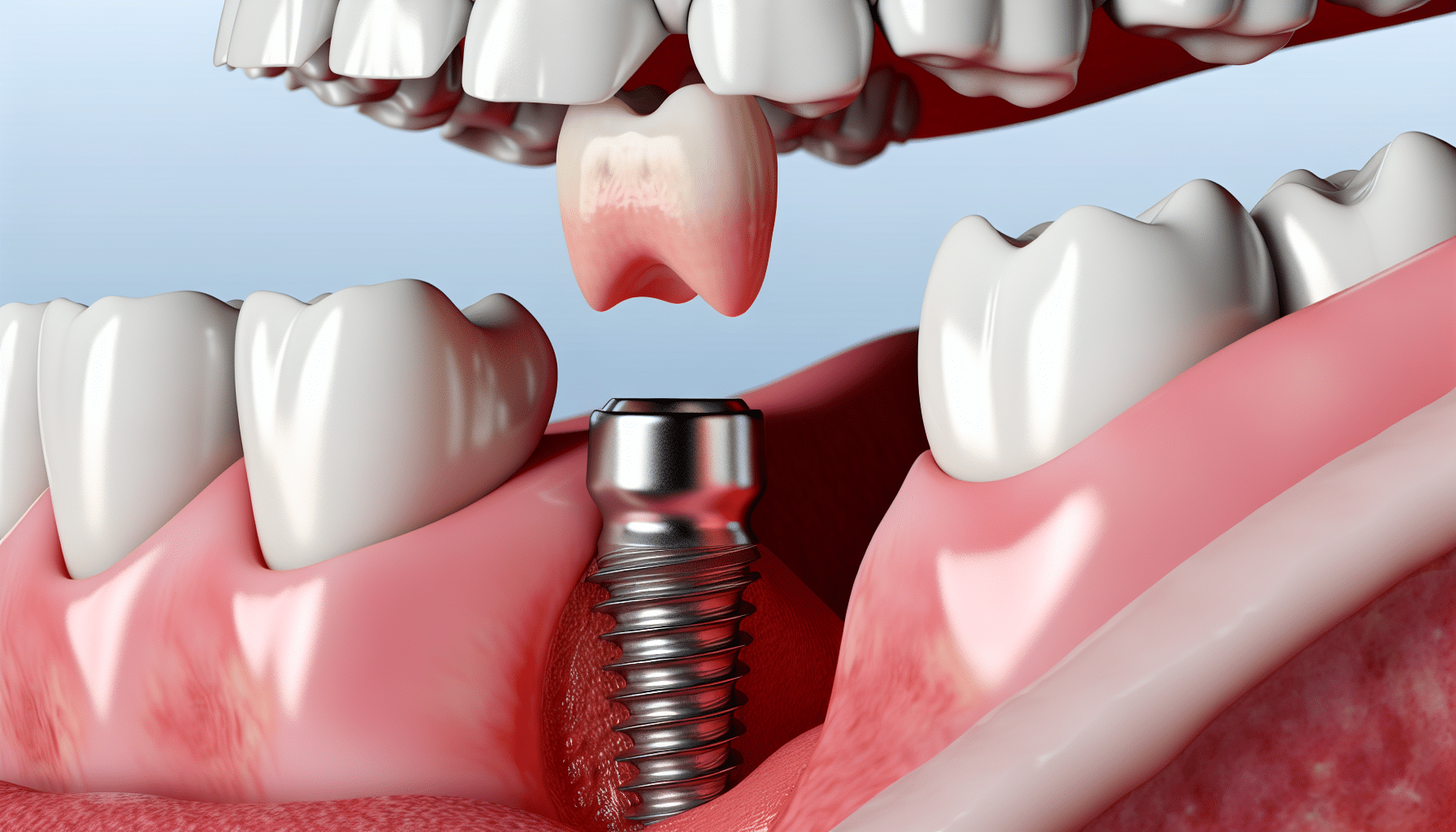
Dental implants replace the root parts of the teeth. Artificial crowns, bridgework or removable dentures— tooth replacements that make up the visible (crown) part/s of teeth — are attached to the implants. In between the implant and the crown of a tooth there is often a connector known as an abutment. The success of the whole system is based on the implant’s attachment to bone. Titanium, the metal of which implants are made, is uniquely osteophilic — literally “bone-loving.” It fuses to bone in a process called osseointegration (“osseo” – bone; “integration” – fusion or joining).
Above the bone where the integration process ends, the abutment comes in contact with the gum tissue where it is supported by a connective (i.e. “connecting”) tissue composed of fibers made of a tough material called collagen. The fibers run beneath the surface parallel to the implant ending at the top of the bone. They hold the gum tissues against the implant surface.
At the very top of the implant assembly, the abutment and lower part of the crown attach to the gum (the surface “skin” layer) via a specialized structure known as an epithelial attachment (“epi” – on top; “thele” – nipple). The cells actually attach to the highly polished metal or ceramic, of which the implants are made, by means of microscopic suction pads.
By contrast, a tooth root is attached to the bony socket that surrounds it — by a periodontal ligament (“peri” – around; “odont” – tooth). The ligament is composed of tiny fibers that insert into the bone on one side and into the tooth root on the other. Above the bone, the fibers attach from the tooth into the gum tissue. An implant has no such attachment. Since the whole periodontal ligament has a greater blood vessel supply through which it can bring cells and nutrients, it is more readily able to resist and fight against infection.Cleaning implant-supported tooth replacements is just as important as cleaning natural teeth, as both depend on healthy surrounding tissues for support. Bacterial biofilm (plaque) collects on implant crowns just as it does on natural teeth, and must be removed on a daily basis at home. Without daily biofilm removal, infection can develop known as peri-implantitis (“peri” – around; implant “itis” – inflammation), which can result in loss of the attachment described above. Unlike inflammation around teeth, this reaction can be quite catastrophic both in rate and amount, quickly leading to a well- or dish-shaped loss of bone around an affected implant. Bone loss can rapidly progress to loss of the implant.
The dental hygienist has an important role to play in keeping dental implants infection-free, and there are many factors to be considered in selecting the right instruments for a professional cleaning. They include: the nature of the debris, meaning whether soft (biofilm, foods) or hard (calculus or tartar, calcified material); the location of the deposits; the type of surface on which they accumulate; and the stubbornness with which they adhere.Your hygienist must select instruments for cleaning that will not damage the crown, abutment, or the implant itself. Maintaining the highly polished, smooth surface of the abutment and crown are critical. If they are scratched they can attract and harbor bacteria. That’s why the instruments used, called scalers and curettes, are most often made of plastics and resins. Natural teeth don’t scratch in the same way, and therefore metal instruments can be used to clean them.
A number of power (ultrasonic) instruments have nylon or plastic sheaths or tips to minimize implant damage. They clean by using high-frequency vibration, which may be necessary if large quantities of debris have accumulated. They are used on a low power setting with a lot of water irrigation, and sometimes antibacterial solutions, to clean and flush material.
If any part of the implant body (root replacement portion) itself is visible, this may mean there is infection that has resulted in gum and/or bone loss. The implant surface becomes exposed following loss of its fusion to the bone. Implant surfaces are generally microscopically “roughened” to increase surface area for bone attachment. But this surface roughness makes implants difficult if not impossible to clean and disinfect. Additionally, some implants are screw-shaped and their threads just add to the cleaning dilemma.
Brushes are used to clean biofilm from exposed areas of an implant wherever possible. If calculus or dental cement (used to secure the crowns) is present on an implant surface, the hygienist needs to use instruments that are effective in removing these contaminants. In such cases the clinician must ensure no scratching or damage is caused by completing the task.
Despite these special cleaning challenges, implants are highly successful. In fact, studies indicate long-term success rates well over.
However, the prevention of peri-implant disease is fundamental to implant health, maintenance and function. And cleaning implants and their related components is an important part of success. Your question indicates that your hygienist is on top of it.